COVID-19 Variants and Outbreaks Prioritisation -- Patient and Public Involvement and Engagement

Outbreak Data Analysis Platform COVID-19 Variants and Outbreaks Prioritisation – Patient and Public Involvement and Engagement
Sinduja Manohar, April 2022
Seeking patient and public insights to prioritise questions on COVID-19 variants and outbreaks
The purpose of the Outbreak Data Analysis Platform is to provide an accessible and usable data resource to enable research that is relevant to COVID-19, including new future COVID-19 outbreaks as well as those arising from other viruses. This will accelerate scientific understanding of new outbreaks for the benefit of patients and the protection of the public. To enable this to happen the Outbreak Data Analysis Platform (ODAP) brings together data from clinical records, research studies and audit data. ODAP is supported by UKRI and the Data and Connectivity Programme of the National Core Studies.
The ODAP management group identified the need to involve patients and the public to provide guidance, challenge and advice. Following a planning workshop with members of the ODAP management group, Data and Connectivity programme staff, and a separate follow-up consultation with a public partner, recommendations were put forward on ways in which to involve patients and the public. One such recommendation was to run a prioritisation consultation with patients and the public to understand their needs and wants.
Understanding public perceptions on research priorities using ODAP data
To ensure that public benefit at is forefront and that this work is shaped and directed by patients and the public, it was agreed that an online prioritisation consultation with patients and the public would run to understand what the research priorities are for patients and the public based on areas of research the ODAP team and research community put forward. By asking patients and the public to prioritise the research questions put forward, the aim is to understand which are urgent, which are ‘nice-to-have’ and to gather any other additional insights and suggested priorities from a patient and public perspective.
216 complete responses were received between 3 March – 8 April 2022
When asked to identify whether they identified as being a patient, member of the public or having COVID (both confirmed and not confirmed with a test), many respondents chose multiple options. For the purpose of analysis, where multiple choices had been selected, individual responses were categorised as:
-
Extremely Clinically Vulnerable > Had COVID-19 > Patient (unrelated to COVID) > Member of the public.
-
For example, if an individual states they were a patient (unrelated to COVID) but also had COVID-19 in the past, for the purposes of analysis they have been categorised only as someone who has had COVID-19.
The order of categorisation was suggested by our public partners to aid analysis and was chosen based on factors they believe to be potentially influential to an individual’s response to the prioritisation consultation.
As such:
-
48 people self-identified and were subsequently categorised as considered extremely clinically vulnerably from COVID-19 and were advised to shield.
-
55 people self-identified and were subsequently categorised as having had COVID-19 (both confirmed and not confirmed with a test)
-
33 people self-identified and were subsequently categorised as being a patient or carer (unrelated to COVID-19)
-
80 people self-identified and were subsequently categorised as being a member of the public
To gain an understanding of who has completed the prioritisation consultation to help determine where there may be gaps and identify specific groups and populations that need more targeted involvement, respondents were asked to self-report their gender, ethnicity, year of birth and geographical location. These were optional questions and there are a handful of respondents who did not wish to disclose their anonymous demographics.
Gender:
-
107 individuals identified as being female
-
100 individuals identified as being male
-
4 individuals identified as being non-binary
Age: Table 1: Respondents were asked to provide their Year of Birth which was then categorised into the following groups
| 16-25 years | 26-35 years | 36-45 years | 46-55 years | 55-65 years | 66-75 years | 76-85 years | 86 years and over |
|---|---|---|---|---|---|---|---|
| 2 | 9 | 19 | 24 | 58 | 68 | 29 | 3 |
Geographical Location: Figure 1 provides an overview of number of respondents from each of the four nations.

The majority of respondents were from England with small levels of representation from Scotland, Wales and Northern Ireland.
Prioritising Research Questions – Theme Areas
A handful of research questions have been put forward by the ODAP team and research community where it is of importance to explore. These questions can be categorised into three main key themes:
-
Theme 1 - How a COVID-19 variant is created and spreads (Q1 in Figure 2)
-
Theme 2 - What determines how unwell a person gets with COVID-19 (Q2 in Figure 2)
-
Theme 3 - How well vaccines and treatments work against COVID-19 (Q3 in Figure 2)
Table 2: Number of people to have ranked each research area
| Rank | Theme 1 - How a COVID-19 variant is created and spreads | Theme 2 - What determines how unwell a person gets with COVID-19 | Theme 3 - How well vaccines and treatments work against COVID-19 |
|---|---|---|---|
| 1 | 62 | 56 | 98 |
| 2 | 47 | 87 | 82 |
| 3 | 107 | 73 | 36 |
Key Findings:
-
Overall, patients and the public are keen to understand ‘how well vaccines and treatments work against COVID-19’.
-
Whilst the categorised populations groups were fairly consistent with each other in terms of how they ranked the research theme areas, it is worth noting those who were deemed ‘extremely clinically vulnerable still prioritised ‘how well vaccines and treatments work against COVID-19’ as most important but this was very closely followed by ‘what determines how unwell a person gets with COVID-19’. Given their pre-disposition to a more severe reaction to COVID-19, this correlates with what we would expect to see.
Figure 2: Research theme areas ranked as ‘1’ broken down by four population groups (percentage) - those who have had COVID-19, those who are deemed extremely clinically vulnerable, patient and public.
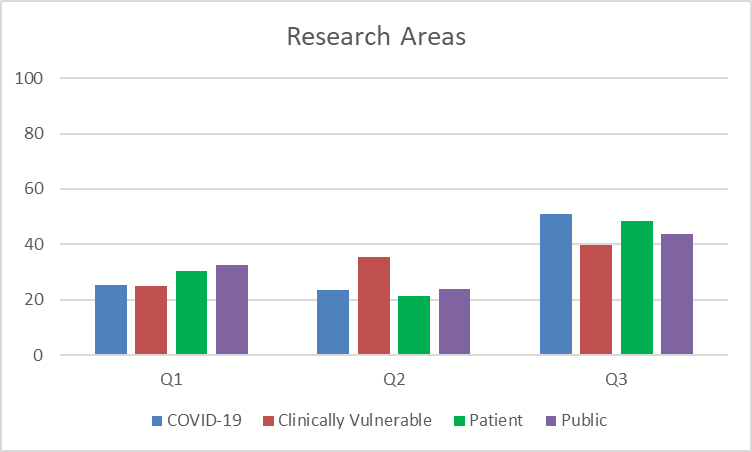
Additional Findings:
-
Findings were fairly consistent in rankings amongst ethnicities although a higher percentage of those who identified as any ethnicity other than ‘White’ prioritised ‘how well vaccines and treatments work against COVID-19’ compared to those who identified as ‘White’ or ‘White British’ (60% compared to 45%).
-
Those aged 56 – 65 years had given equal priority to ‘how well vaccines and treatments work against COVID-19’ as well as ‘how a Covid-19 variant is created and spreads’.
-
Whilst females strongly prioritised ‘how well vaccines and treatments work against COVID-19’ (48%), men had split their prioritisation with equal weighting given to ‘how a Covid-19 variant is created and spreads’ and ‘how well vaccines and treatments work against COVID-19’.
-
All four nations had prioritised ‘how well vaccines and treatments work against COVID-19’. Those in England has then put ‘what determines how unwell a person gets with COVID-19’ has a close second in their prioritisation whilst this was deemed quite low in the other three nations.
How a COVID-19 variant is created and spreads - Prioritising Questions
A handful of research questions have been put forward by the ODAP team and research community where it is of importance to explore. Two questions were put forward under this theme:
-
Why do different variants of COVID-19 have different abilities to transmit between people, whether that is more or less easily? (Q1 in Figure 3)
-
COVID 19 variants can change if they infect people whose immune system (our body’s way of fighting infection) doesn’t work. How and why does this happen? (Q2 in Figure 3)
Table 3: Number of people to have ranked each individual research question
| Rank | Why do different variants of COVID-19 have different abilities to transmit between people, whether that is more or less easily? | COVID 19 variants can change if they infect people whose immune system (our body’s way of fighting infection) doesn’t work. How and why does this happen? |
| 1 | 114 | 102 |
| 2 | 102 | 114 |
Key Findings:
-
Overall, patients and the public are keen to understand ‘why different variants of COVID-19 have different abilities to transmit between people, whether that is more or less easily?’.
-
However, it is worth noting that the overall differences in ranking was quite small and not a significant level of differentiation.
-
Looking more closely at the categorised populations groups in Figure 3, it is worth noting those who were deemed extremely clinically vulnerable had instead prioritised ‘COVID 19 variants can change if they infect people whose immune system (our body’s way of fighting infection) doesn’t work. How and why does this happen?’. Given their pre-disposition to a more severe reaction to COVID-19, this correlates with what we would expect to see.
Figure 3: Research questions under ‘how a COVID-19 variant is created and spreads’ theme ranked as ‘1’ broken down by four population groups (percentage) - those who have had COVID-19, those who are deemed extremely clinically vulnerable, patient and public.
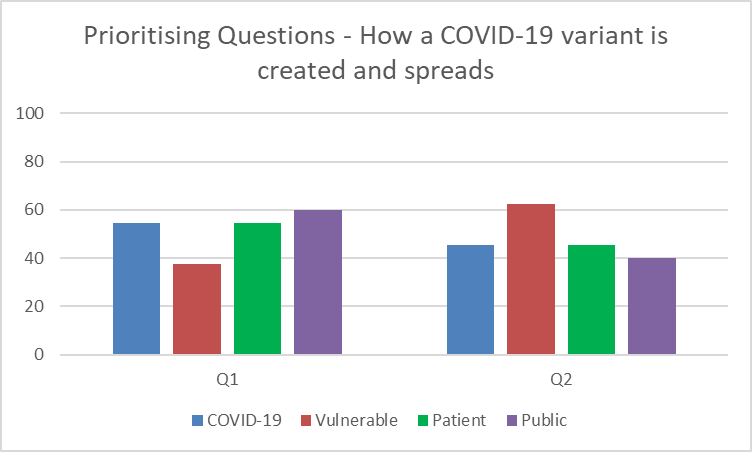
Additional Findings:
-
Whilst rankings were relatively similar amongst those who identified as ‘White’, ‘White British’ or ‘White Other’, those who identified as being any other ethnic minority have strongly prioritised ‘Why do different variants of COVID-19 have different abilities to transmit between people, whether that is more or less easily?’ with 83% highlighting it as an area of importance.
-
Rankings amongst different age groups are consistent with the overall findings (around 50% for each research question) except for those aged 35 and under who had a much stronger preference for exploring ‘COVID 19 variants can change if they infect people whose immune system doesn’t work. How and why does this happen?’ – 100% of those aged 16–25 and 78% of those agenda 26-35 years.
-
Across those who identify as males, females and non-binary, findings were consistent with the overall findings – around 50% for each research question
-
Those in England and Wales correlate with the overall findings (although slightly higher percentage of 55%). However, those in Scotland and Northern Ireland strongly prioritised exploring ‘COVID 19 variants can change if they infect people whose immune system doesn’t work. How and why does this happen?’ (66% and 68% respectively).
What determines how unwell a person gets with COVID-19 - Prioritising Questions
A handful of research questions have been put forward by the ODAP team and research community where it is of importance to explore. Three questions were put forward under this theme:
-
Do different COVID-19 variants cause more or less severe disease? (Q1 in Figure 4)
-
Do a person’s genes affect the way they respond to different COVID 19 variants? (Q2 in Figure 4)
-
Why do some people develop Long COVID – while others don’t? (Q3 in Figure 4)
Table 4: Number of people to have ranked each individual research question
| Rank | Do different COVID-19 variants cause more or less severe disease? | Do a person’s genes affect the way they respond to different COVID 19 variants? | Why do some people develop Long COVID – while others don’t? |
| 1 | 75 | 63 | 78 |
| 2 | 62 | 79 | 75 |
| 3 | 79 | 74 | 63 |
Key Findings:
-
Overall, patients and the public were relatively even in ranking questions under this research theme with two questions ranking very similarly in terms of importance - ‘do different COVID-19 variants cause more or less severe disease?’ and ‘why do some people develop Long COVID – while others don’t?’.
-
However, it is worth noting that the overall differences in ranking was quite small and not a significant level of differentiation.
-
Looking more closely at the categorised populations groups in Figure 4, it is worth noting those who were deemed extremely clinically vulnerable had more strongly prioritised exploring whether ‘different COVID-19 variants cause more or less severe disease?’. Given their pre-disposition to a more severe reaction to COVID-19, this correlates with what we would expect to see. Additionally, although minimal, those who were categorised as members of the public had a slightly stronger preference to exploring research around ‘why some people develop Long COVID – while others don’t’ (8% higher).
Figure 4: Research questions under the ‘what determines how unwell a person gets with COVID-19’ theme ranked as ‘1’ broken down by four population groups (percentage) - those who have had COVID-19, those who are deemed extremely clinically vulnerable, patient and public.
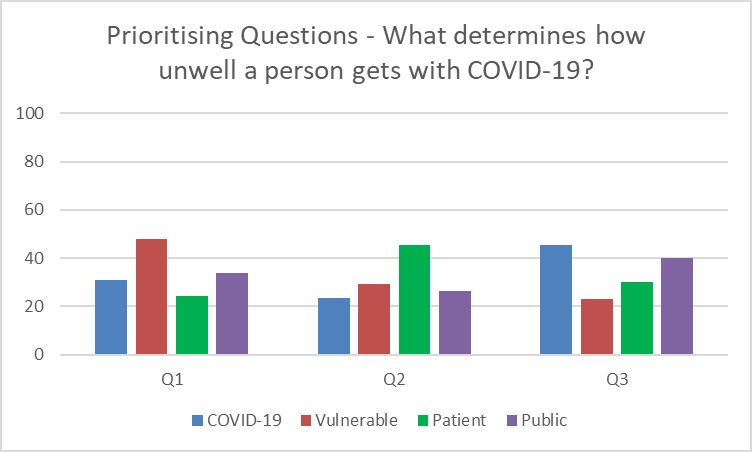
Additional Findings:
-
Whilst overall there were relatively small differences in priorities of research questions under this theme, those who identified as being any other ethnic minority have strongly prioritised exploring whether ‘a person’s genes affect the way they respond to different COVID 19 variants?’ with 67% highlighting that as an area of importance. Given the differences we have seen through the pandemic of how COVID-19 affects particular ethnic minorities, this finding would correlate with what we would expect to see.
-
Although the overall findings showed the two questions - ‘do different COVID-19 variants cause more or less severe disease?’ and ‘why do some people develop Long COVID – while others don’t?’ ranked very similarly in terms of importance, there is a much higher differentiation when exploring differences based on age groups – with those aged 26-35 and 36-45 sharing that research into why ‘some people develop Long COVID – while others don’t?’ was nearly 50% more important than whether ‘different COVID-19 variants cause more or less severe disease?’ in these two age groups.
-
When exploring research questions of importance separated by gender, the differences in ranking were more significant. Men prioritised finding out whether ‘different COVID-19 variants cause more or less severe disease?’ (40%) whilst women put importance on understanding ‘why some people develop Long COVID – while others don’t?’ (43%). Those who identify as non-binary wanted to understand whether a ‘person’s genes affect the way they respond to different COVID 19 variants?’ (75%). Given these are significant differences to the overall findings, it would be of use to explore the reasons behind it.
-
Those in England, Wales and Norther Ireland correlate with the overall findings. Whilst the priority question remained the same, those in Scotland placed stronger importance in understanding ‘why some people develop Long COVID – while others don’t? – nearly 50% of the population placed this as more important than the other two questions combined.
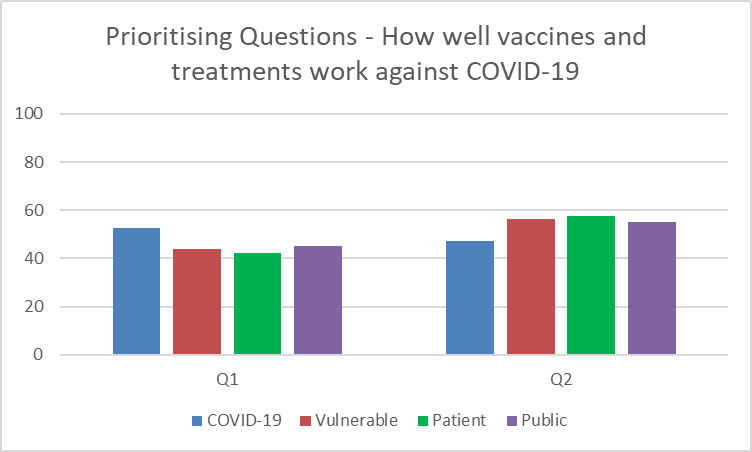
How well vaccines and treatments work against COVID-19 - Prioritising Questions
A handful of research questions have been put forward by the ODAP team and research community where it is of importance to explore. Two questions were put forward under this theme:
-
Do different COVID-19 variants need different treatments? (Q1 in Figure 5)
-
How does the body’s immune response to vaccination differ depending on the COVID-19 variants? (Q2 in Figure 5)
Table 5: Number of people to have ranked each individual research question
| Rank | Do different COVID-19 variants need different treatments? | How does the body’s immune response to vaccination differ depending on the COVID-19 variants? |
| 1 | 100 | 116 |
| 2 | 116 | 100 |
Key Findings:
-
Overall, patients and the public are keen to understand ‘how the body’s immune response to vaccination differs depending on the COVID-19 variants?’.
-
However, it is worth noting that the overall differences in ranking was quite small and not a significant level of differentiation.
-
Looking more closely at the categorised populations groups in Figure 5, the way in which the different categorised population groups has ranked between the two questions is fairly consistent with the overall findings.
-
There is, however, about a 10% increase in the proportion of those who have had COVID-19 who would instead prioritise understanding whether ‘different COVID-19 variants need different treatments?’ Given these are individuals who have had COVID-19 themselves, they may be considering research in the future that could help them overcome the symptoms they experienced and is something in their control (unlike how the body’s immune response differs which is outside of anyone’s control).
Figure 5: Research questions under ‘how well vaccines and treatments work against COVID-19’ theme ranked as ‘1’ broken down by four population groups (percentage) - those who have had COVID-19, those who are deemed extremely clinically vulnerable, patient and public.
Additional Findings:
-
Whilst overall there were relatively small differences in priorities of research questions under this theme, those who identified as being any other ethnic minority have strongly prioritised exploring how the ‘body’s immune response to vaccination differs depending on the COVID-19 variants ‘with 63% highlighting that as an area of importance. Given the differences we have seen through the pandemic of how COVID-19 affects particular ethnic minorities, this finding would correlate with what we would expect to see.
-
Findings across genders and locations across the UK were consistent with the overall prioritisation for the two research questions under this theme.
-
Additionally, findings across age groups were also consistent with the overall prioritisation except for those aged 16-25 and 26-35 where 75% and 76% of those age groups respectively prioritised understanding ‘how the body’s immune response to vaccination differ depending on the COVID-19 variants?’. Although the same question has been prioritised there is a significant difference on the level of importance placed on this question.
Research Areas and Questions put forward by patients and the public
Throughout the online consultation, respondents were provided with opportunities to suggest additional research questions or areas of focus. 189 comments and questions were received, some of which are specific to the work of ODAP and others that are more general to COVID-19 research yet still of tremendous use and value to the wider research question. After removing duplicates and general comments, including re-emphasising the importance of questions already prioritised, the questions and comments fall under the following themes:
Effect of variants:
-
Can we predict future variants based on the variants that have emerged so far? Why are some variants more infectious than others?
-
Will it be more beneficial to enable different isolation periods for different variants?
-
The ability of variants to make individuals more susceptible to re-infection
-
How mutations develop and if/how to prevent development of more resistant and harmful strains
-
To what extent variants is linked to severity of disease in particular populations and/or conditions
-
Effects of variants on main organs
-
Extent to which variants impact likelihood and severity of Long COVID
-
Extent to which variants impact different ethnic minorities
Severity of COVID-19 symptoms
-
What determines the severity of COVID symptoms (beyond what was asked in the survey)?
-
The effects of co-morbidities on how unwell a person is likely to be with COVID-19
-
To what extent underlying health conditions (e.g., heart failure or neurological conditions) affects how a person reacts to COVID-19 and which conditions in particular have more of an effect than others
-
Who remains vulnerable to severe effects of COVID-19?
-
Does it affect certain age groups, genders, ethnicities etc more than others? If so, why?
-
Exploring gender differences between reactions to COVID-19 and treatment regimes
-
Effect of medication on severity of disease
-
Whether overall fitness prevents severe disease to COVID-19 and to what extent
-
Whether any diets, supplements etc have shown to lead to a better response to COVID-19 infection
Long COVID:
-
What puts people at a higher risk of Long COVID?
-
Ways in which to avoid and prevent Long COVID, e.g., either by the speed with which we are able to recognise and treat COVID infection, or by the way in which we target treatment for infection
-
Long-term impact of Long COVID and if/how vaccination enables reduction of impact
-
How well treatments work against Long COVID
a. How well treatments work against differing Long COVID symptoms
Transmission:
-
Factors affecting transmission that go beyond the response of the immune system.
-
Role of genes in being more susceptible to transmission of the virus
-
Does air quality have an impact on transmission?
Vaccinations:
-
Likelihood and effectiveness of a regular, e.g., yearly COVID vaccination (as with the flu vaccination)
a. How well protected am I 6 months on from my booster jab?
-
Usefulness of vaccines especially for those on immunosuppressants
-
Does the vaccine protect people with a compromised immune system?
-
Side effects of vaccines and severity of impact
-
Understanding what factors lead to sever COVID-19 symptoms and whether vaccinations could target these specific factors
-
Exploring the development of longer-term vaccines that negate the need for boosters
-
Factors the affect the length of cover vaccinations can provide
Other:
-
What does COVID becoming endemic really mean?
a. Will COVID get less severe?
-
Understanding the data behind the proportion of those who are asymptomatic
-
Will those who are asymptomatic have ‘hidden’ damage that could cause issues later in life?
Limitations of Approach and Recommendations
A benefit to running an online prioritisation consultation is that it enables a larger number of patients and the public to get involved without it taking too much of their time whilst still enabling a great deal of insights.
To enable as many people as possible to complete the prioritisation exercise, it was shared with a wide range of patient and public networks including those who are not familiar with health data research. Whilst a pre-read was provided, an option to have a call with the team for additional information was given and the information and questions were as accessible as possible, it still led to a number of questions and areas of confusion by those who got involved. A handful of comments highlighted “couldn’t understand the difference between the two questions” when prioritising research questions and led to patients and the public putting forward areas of research that would not be relevant to the work of ODAP (although still useful to have and share more widely with the research community).
A recommendation to improve on this would be to hold small workshops with patients and the public where the team would be able to explain the work of ODAP in more detail and have more in-depth discussions on different areas of work to better understand areas of priority and wishes for future research. This will also enable a wider range of research questions to be developed – having a small number of questions in the original consultation has meant that where there is not a strong preference for only one particular question, it means insights can be more difficult to obtain given there are only two or three questions to choose from.
Not unique to this particular prioritisation consultation, there is a lack of diversity in terms of the people who got involved, particularly when it comes to ethnicity and ages. Whilst there was a fairly even split between males and females, there were significantly fewer people getting involved who were below 45 and were from ethnic minorities. However, the results showed that patients and the public from these groups and populations had differing views and opinions compared to those who were older and were ‘White’ and/or ‘White British’ respectively. The same could also be said to enabling more people who have had COVID-19 or are deemed to be extremely clinically vulnerable to get involved.
As such, a recommendation would be to further develop understanding of priorities from a diverse population by running a more targeted prioritisation consultation. However, this can only be achieved with more time and resource behind it given the resource needed to build and cultivate relationships with these groups and populations and ensure the method taken suits their needs and preferences (e.g., instead of a survey they may prefer focus groups etc).